Abstract
Over the past few decades, antimicrobial resistance (AMR) has shaped up to be one of the most important and crucial global health issues, and countries like Bangladesh, which have poor and weak health care systems are at the highest risk. Lack of awareness and insufficient knowledge about AMR, inappropriate usage of antimicrobial medicines, and inadequate supervision regarding the sale and usage of antimicrobial drugs are aggravating the situation. It would be impossible to tackle the worsening AMR situation in Bangladesh unless the mentioned issues are addressed and effective measures are taken to improve the overall health care system of the country.
Introduction
Antimicrobial resistance occurs when microorganisms (such as bacteria, fungi, viruses, or protozoa) are able to neutralize the effects of antimicrobial medications, rendering them useless. This ability to nullify the action of antimicrobial medicine is not an inherent characteristic of the microbes, rather it is developed over time. According to the World Health Organization (2021), the mistreatment and overuse of antimicrobials, lack of access to safe water, sanitation, and hygiene, along with inadequate infection and disease prevention and control in healthcare institutions, and farms are the major causes of antimicrobial resistance. Even though a large number of factors are responsible for this, the overuse and wrong application of antimicrobial medicines serve as the main driving force behind this exponential rise in AMR cases in recent years (WHO, 2021). Each year nearly 700,000 preventable deaths are directly linked to AMR and this number is projected to rise exponentially and cross 10 million deaths annually by the end of 2050 as stated in a report by O’Neill (2016).
South-east Asia is one of the most vulnerable regions and possesses the highest risk when it comes to AMR and Bangladesh is no different (Chereau et al., 2017). According to a report published by Jasim (2019), cases related to AMR in Bangladesh is on the rise throughout the last few years and experts suggest that there will be an exponential rise in the near future if the present situation is left unnoticed. According to data from the Bangladesh Society of Anesthesiologists (2013), the percentage of patients admitted to Bangabandhu Sheikh Mujib Medical University Hospital (BSMMU) ICU showing the signs of multi-antibiotic resistance is 52% and the number is rapidly growing. Thus, it has become an absolute necessity to raise awareness about AMR in Bangladesh and control the situation before it gets out of grasp.
Assessment of the Situation in Bangladesh
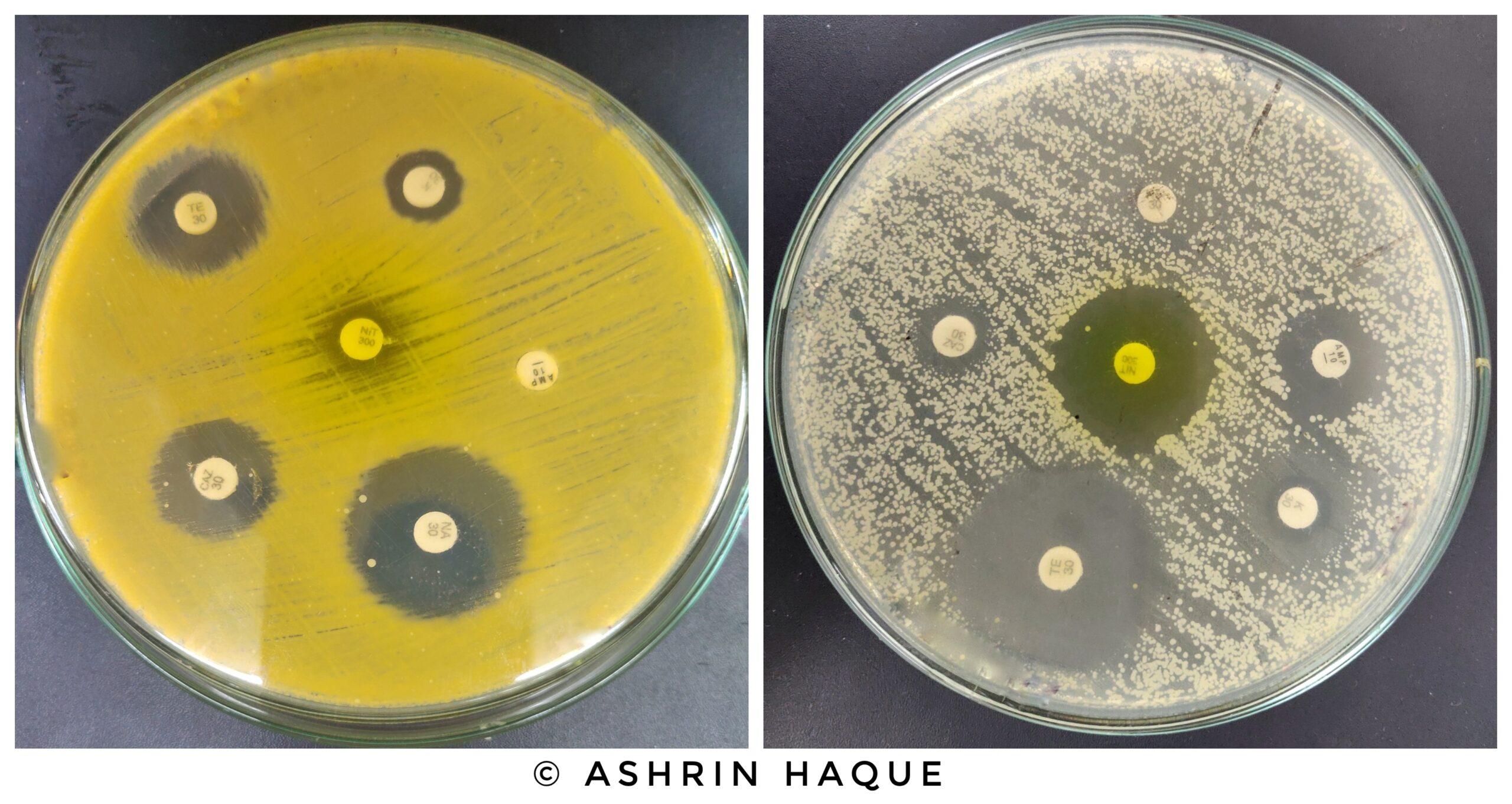
Various factors are responsible for the current state of antimicrobial resistance in Bangladesh. Jasim (2019) in his report, pointed out, most of the health officials and physicians in the country suggest that apart from the overuse and inappropriate application of medicines, the lack of enforcement of legislative regulations plays a vital role in the increment of AMR in Bangladesh. Despite having laws that prohibit the sale of antibiotics without a valid prescription by a doctor, most pharmacies in the country continue to sell different antibiotic and antimicrobial medicines over-the-counter (OTC) without any valid prescription (Darj et al., 2017). In addition, according to a recent research article published by Hoque et al. (2020), the prevalence of self-treatment and the tendency of administering drugs on their own by the patients without the prescription of a registered physician is dangerously high in Bangladesh. The article concluded that the percentage of people consuming some form of medicine without consulting a doctor is 36% for food poisoning, 28% for the common cold, and 13% for presumed infections; among which only 17.5% of people have knowledge about antibiotics. The overuse and misuse of certain antibacterial drugs have caused various bacteria like Escherichia coli, Streptococcus aureus, Pseudomonas aeruginosa, and Klebsiella pneumoniae to become highly resistant to antibiotic medicines. For instance, 86% of E. coli bacteria collected from urine samples from hospitals of Dhaka showed a high level of resistance towards amoxicillin and ceftazidime, two well-known antibiotics (Hasan, 2019). On the other hand, similar kinds of drug-resistant bacteria can also enter the human body through the consumption of poultry, fish, and meat. Studies conducted by a group of researchers of the Chittagong Veterinary and Animal Sciences University (CVASU) conclude that more than 19 types of antibiotics are used in poultry farms and fisheries all over the country. This has led to 54.55% of broiler chickens carrying one or more multi-drug resistant bacteria (Khan et al., 2020).
As antimicrobial resistance has turned into a major health issue in Bangladesh, immediate actions have to be taken. Firstly, mass awareness has to be raised about the present condition of AMR in Bangladesh and how it will affect the future, as only 17.5% of people in Bangladesh who regularly consume some forms of antimicrobial drugs are aware of the adverse effects of AMR as stated by Hoque et al. (2020). Secondly, strong legislative actions should be taken to stop the sale of antibiotics and antiviral medicines unless a valid prescription by a certified physician is presented. Thirdly, and most importantly, the medical infrastructure of the countries should be improved and diagnostic procedures should be developed and effectively utilized so that the pathogen responsible for the infection is identified accurately and medications are suggested accordingly. Successful monitoring and execution of these steps will help to minimize the risk of AMR in Bangladesh.
Conclusion
To conclude, as the AMR situation is worsening and more species of microbes are exhibiting signs of anti-microbial resistance in Bangladesh, it is of utmost importance that mass awareness programs are initiated along with strict regulatory methods and supervision. Awareness is at the forefront when it comes to eradicating AMR as most of the factors that lead to the development of drug resistance in microbes are linked to a lack of awareness among people. If the mass population comes to know about the adverse effects of antimicrobial resistance, it would be easier to control infectious diseases and the misuse of antimicrobial medicines could be reduced.
References:
- Chereau, F., Opatowski, L., Tourdjman, M., & Vong, S. (2017). Risk assessment for antibiotic resistance in South East BMJ, j3393. https://doi.org/10.1136/bmj.j3393
- Darj, E., Newaz, M. S., & Zaman, M. H. (2019). Pharmacists’ perception of their challenges at work, focusing on antimicrobial resistance: a qualitative study from Global Action Health.https://doi.org/10.1080/16549716.2020.1735126
- Hasan, M. J., Hosen, M. S., & Bachar, S. C. (2019). The resistance growing trend of common gram-negative bacteria to the potential antibiotics over three consecutive years: a single center experience in Bangladesh. Pharmacy & Pharmacology International https://doi.org/10.15406/ppij.2019.07.00240
- Hoque, , Ahmed, S. M., Naher, N., Islam, M. A., Rousham, E. K., Islam, B. Z., & Hassan,(2020). Tackling antimicrobial resistance in Bangladesh: A scoping review of policy and practice in human, animal and environment sectors. PLOS ONE, 15(1), e0227947. https://doi.org/10.1371/journal.pone.0227947
- Jasim, M. M. (2019, November 25). The Bussiness Standard. Retrieved from net: https://www.tbsnews.net/bangladesh/health/52-icu-patients-bsmmu-multi- antibiotic-resistant
- Khan, A., Imtiaz, M.A., Sayeed, M.A. et al. (2020). Antimicrobial resistance pattern in domestic animal – wildlife – environmental niche via the food chain to humans with a Bangladesh perspective; a systematic review. BMC Vet Res 16. https://doi.org/10.1186/s12917-020-02519-9
- Mondal, K., Roy, B. R., Yeasmeen, S., Haque, F., Huda, A. Q., & Banik, D. (2014). Prevalence of microorganism and emergence of bacterial resistance in ICU of the Bangabandhu Sheikh Mujib Medical University of Bangladesh. Journal of the Bangladesh Society of Anaesthesiologists, 26(1), 20–26. https://doi.org/10.3329/jbsa.v26i1.19811
- O’Neill, J. (2016). Tackling drug-resistant infections globally: final report and Government of the United Kingdom. https://doi.org/APO-63983
- World Health Organization. (2021). Retrieved from int: https://www.who.int/news- room/fact-sheets/detail/antimicrobial-resistance
“Since the article has been written to reflect the actual views and capabilities of the author(s), they are not revised for content and only lightly edited to be confirmed with the Learn life sciences style guidelines”









Well done!
Hope to see more writings in future.
Thank you a lot for sharing this with all people you actually understand what you are speaking approximately! Bookmarked. Kindly also discuss with my site =). We will have a hyperlink change agreement among us!
Have you ever considered writing an e-book or guest authoring on other sites? I have a blog based upon on the same information you discuss and would really like to have you share some stories/information. I know my readers would value your work. If you’re even remotely interested, feel free to send me an e-mail.
My brother suggested I might like this blog. He was totally right. This post actually made my day. You can not imagine simply how much time I had spent for this information! Thanks!
I’ve been browsing online more than 3 hours today, yet I never found any interesting article like yours. It is pretty worth enough for me. Personally, if all web owners and bloggers made good content as you did, the net will be a lot more useful than ever before.
Useful info. Fortunate me I found your site by accident, and I am shocked why this twist of fate didn’t took place earlier! I bookmarked it.
Valuable info. Fortunate me I found your web site by accident, and I’m stunned why this coincidence didn’t took place earlier! I bookmarked it.
I really like your writing style, wonderful info, thanks for putting up :D. “Every moment of one’s existence one is growing into more or retreating into less.” by Norman Mailer.
I have read so many posts about the blogger lovers except this
piece of writing is in fact a fastidious post, keep it up.
Hey there I am so glad I found your webpage, I really found you by accident, while I was searching on Digg for something else, Anyways I am here now and would just like to say many thanks for a remarkable post and a all round interesting blog (I also love the theme/design), I don’t have time to look over it all at the moment but I have bookmarked it and also added your RSS feeds, so when I have time I will be back to read a great deal more, Please do keep up the superb work.
I dugg some of you post as I cerebrated they were very helpful invaluable
Cool website!
My name’s Eric, and I just found your site – learnlifescience.com – while surfing the net. You showed up at the top of the search results, so I checked you out. Looks like what you’re doing is pretty cool.
But if you don’t mind me asking – after someone like me stumbles across learnlifescience.com, what usually happens?
Is your site generating leads for your business?
I’m guessing some, but I also bet you’d like more… studies show that 7 out 10 who land on a site wind up leaving without a trace.
Not good.
Here’s a thought – what if there was an easy way for every visitor to “raise their hand” to get a phone call from you INSTANTLY… the second they hit your site and said, “call me now.”
You can –
Talk With Web Visitor is a software widget that’s works on your site, ready to capture any visitor’s Name, Email address and Phone Number. It lets you know IMMEDIATELY – so that you can talk to that lead while they’re literally looking over your site.
CLICK HERE http://boostleadgeneration.com to try out a Live Demo with Talk With Web Visitor now to see exactly how it works.
Time is money when it comes to connecting with leads – the difference between contacting someone within 5 minutes versus 30 minutes later can be huge – like 100 times better!
That’s why we built out our new SMS Text With Lead feature… because once you’ve captured the visitor’s phone number, you can automatically start a text message (SMS) conversation.
Think about the possibilities – even if you don’t close a deal then and there, you can follow up with text messages for new offers, content links, even just “how you doing?” notes to build a relationship.
Wouldn’t that be cool?
CLICK HERE http://boostleadgeneration.com to discover what Talk With Web Visitor can do for your business.
You could be converting up to 100X more leads today!
Eric
PS: Talk With Web Visitor offers a FREE 14 days trial – and it even includes International Long Distance Calling.
You have customers waiting to talk with you right now… don’t keep them waiting.
CLICK HERE http://boostleadgeneration.com to try Talk With Web Visitor now.
If you’d like to unsubscribe click here http://boostleadgeneration.com/unsubscribe.aspx?d=learnlifescience.com
Hey, thanks for the blog.Really thank you! Great.
I must thank you for the efforts you have put in writing this blog. Im hoping to check out the same high-grade blog posts from you in the future as well. In fact, your creative writing abilities has encouraged me to get my own, personal site now 😉
I appreciate you sharing this blog post. Thanks Again. Cool.