Introduction
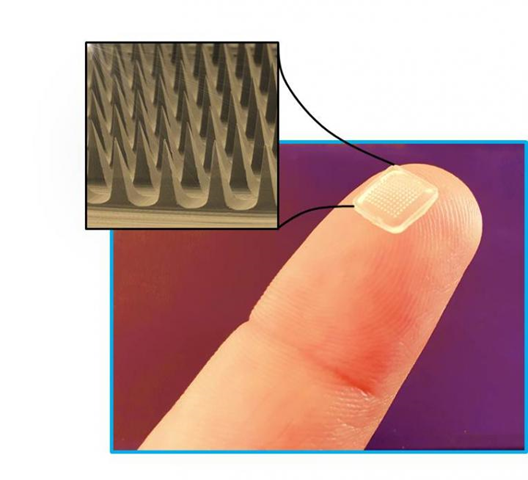
For many years, drug administration orally has become a usual technique of drug delivery because of its ease and lack of invasiveness. This form, however, is only suitable for systemic drugs and has a lot of drawbacks, including poor absorption and high first-pass removal. Drug administration by a needle (e.g., intramuscular, subcutaneous, and intravenous) has been frequently utilized as an alternative to administering a specific dosage in a rapid and regulated way by penetrating the skin with small tubular instruments, but it has eventually resulted in excessive pain and severe skin damage (J. Kim et al., 2018). This suggested that the use of microneedles may be extremely useful, and it has piqued researchers’ interest in the field of microneedles (Zhao et al., 2020). Microneedles are tiny, needle-like projections that are arranged in clusters on surfaces varying from a few square millimeters to many square centimeters in size (Plamadeala et al., 2019).
Why microneedles?
The microneedle procedure is a modernized approach to delivering substances across the skin in an optimal manner since the skin is an absorptive organ that is targeted in the transdermal delivery system (Zhao et al., 2020). It may reach the epidermal layers’ without irritating nerve endings or digging further into the blood vessels of the skin. As a result, MNs are non-invasive and do not cause inflammation or bleeding (Plamadeala et al., 2019) enabling the microneedles approach to be much superior to conventional transdermal methods because of possessing additional benefits such as simplicity and increased patient compliance (Y. C. Kim et al., 2012; Zhao et al., 2020).
Types of microneedles and their mechanisms
Solid, coated, dissolving and hollow microneedles are among the various forms of microneedles that have been fabricated and studied for use in drug distribution.
- Solid microneedles: It builds conduit pathways in the skin, allowing drugs to be delivered later. Drug diffusion across the skin is facilitated by the channels. The drug is taken up by the capillaries, resulting in a systemic effect. It may also be used for a local effect. Biodegradable polymer solid microneedles have the adequate mechanical strength to pierce the stratum corneum and improve drug absorption. The downside of the solid microneedle is that the formed channel must be closed to prevent unnecessary material or contaminants from being transported (Waghule et al., 2019; Sharma et al., 2019).
- Hollow microneedles: It has an opening on the tip of the needle and a hollow space inside that can hold medications. They have the ability to administer medications directly to the epidermis or upper dermis membrane. These microneedles are particularly well-suited to delivering high-molecular-weight compounds such as vaccines, oligonucleotides, and proteins. They can be helpful when administering massive doses of medication. To develop a hollow microneedle, it’s critical to maintain pressure, sharpness, and precise drug flow (Waghule et al., 2019).
- Dissolving microneedles: They are biodegradable polymer-fabricated microneedles that contain drug encapsulation. Once the microneedles are inserted into the skin, they dissolve. It has higher bio usability and the needles dissolve quickly, making it one of the better microneedle options. Within the skin, a degraded polymer regulates drug release. Dissolving microneedles have the downside of taking longer to dissolve and making complete penetration difficult. When designing dissolving microneedles, effective needle drug delivery is a critical aspect that faces challenges. As a result, polymer-drug mixing is an essential step in the fabrication process (Waghule et al., 2019; Koh et al., 2018).
- Coated microneedles: A soluble drug coating is applied to coated microneedles. They have rapid drug release by dissolving the needles’ coating layers. The amount of drug used is determined by the thickness of the coating film. The needles are usually very small (Waghule et al., 2019).
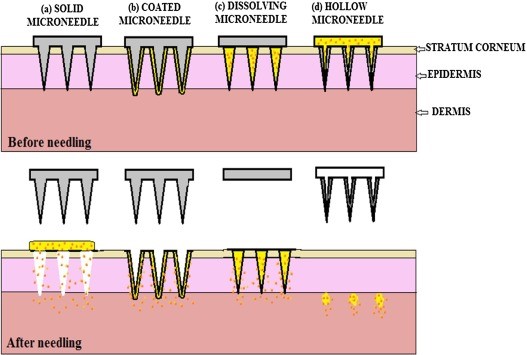
Figure. Different types of microneedles (Waghule et al., 2019).
Applications
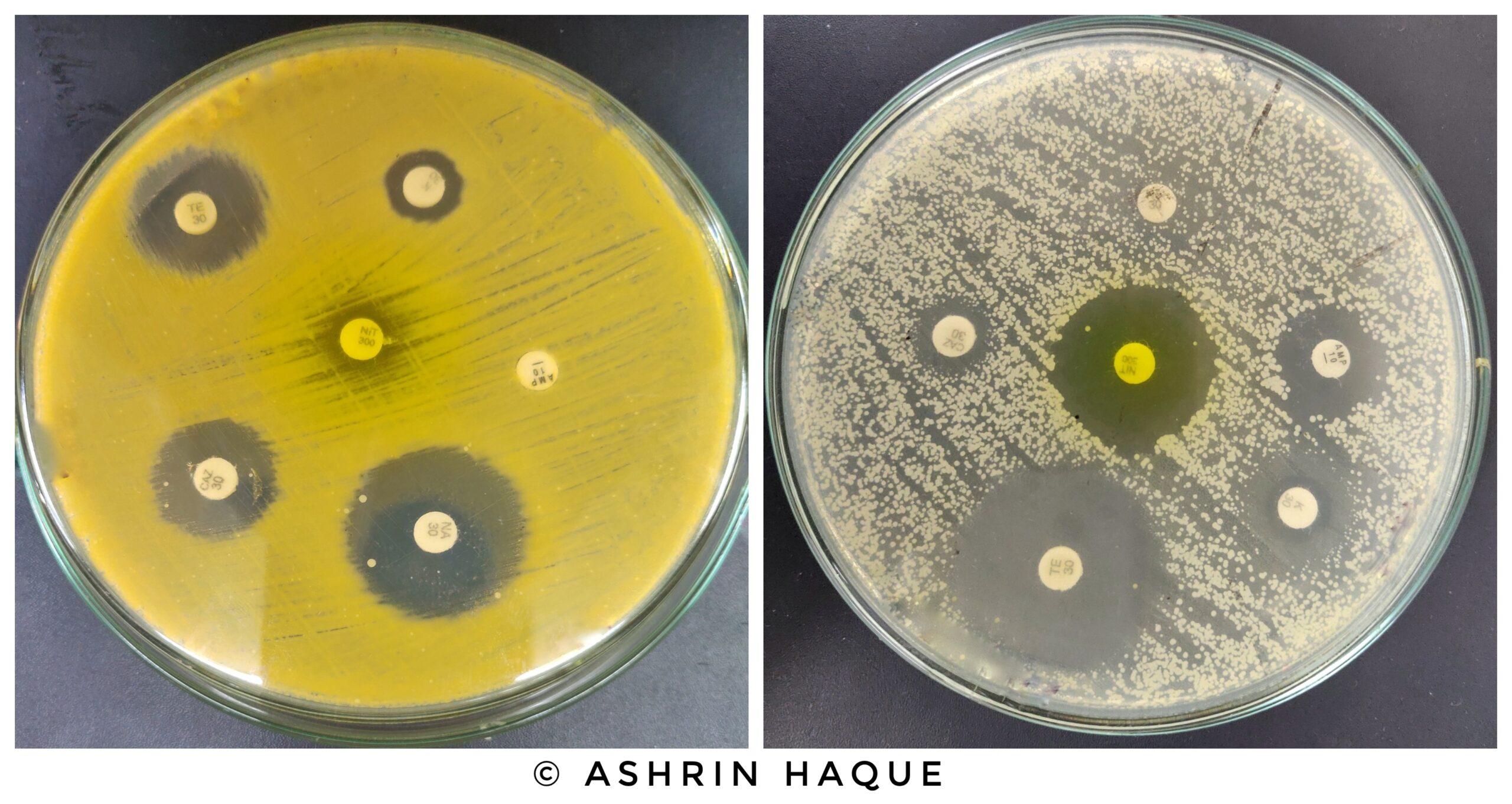
- Vaccines: The administration of vaccinations is one of the most promising uses for microneedles. Some vaccines are lyophilized, diluted, and administered more than once, all of which raise costs, and waste and increase the chance of contamination during delivery and storage. In addition to lowering expenses, the higher immune-responsive microenvironment found in skin tissues, as opposed to subcutaneous and muscular tissues, makes microneedles more efficient in delivering vaccines. Viral vectors, DNA, protein, peptide, virus-like particles, nanoparticle vaccines, and attenuated or inactivated viruses have all been effectively administered using microneedles. In light of the present COVID-19 pandemic, to assess the immunogenicity of the recombinant SARS-CoV-2 S1 vaccine, COVID-19 mice were given a percutaneous injection of the vaccine. It was discovered that 2 weeks after vaccination, soluble microneedles carrying the vaccine induced a potent antigen-specific antibody response (Xu et al., 2021).
- Cancer Therapy: Microneedle treatment has been investigated as a way to administer anti-cancer drugs or to elicit anticancer immunologic responses using anti-cancer antigens, immunological adjuvants, or genetic material (e.g. drugs and nanoparticles). In that approach, the local application of microneedle-based devices can boost the distribution and the amount of medication that reaches the deeper parts of the tumors, while reducing the treatment leakage to neighboring tissues and the adverse effects (Xu et al., 2021).
- Diabetes Therapy: A painless, non-invasive, and repeatable self-administration approach is urgently needed due to long-term consequences and poor compliance with frequent insulin injections. Even more crucially, the dose should be changed to meet the actual need. These issues can be resolved by MNs since they act as a minimally invasive skin interface technique. Furthermore, microneedles can prevent gastrointestinal discomfort and first-pass effects via oral administration because they are a transdermal drug delivery technique. It has been demonstrated that administering insulin through an MN lowers glucose levels, with positive outcomes in animal models. In trials, 0.05–0.5 units of insulin administered using MN technology resulted in a decrease in glycemic levels of around 47%–80% (Jana & Wadhwani, 2019).
- Wound Healing: After being destroyed by various causes of injury, the process of wound healing involves the regeneration of the original skin structure. Microneedles arrays (MAs), which have a high specific surface area and the potential to deliver drugs transdermally, are now known to be promising biomaterials for wound healing. Due to their painless and less intrusive qualities, MAs are often utilized in the healing of wounds. Microneedle arrays may penetrate the adverse environment on the wound surface, such as vascular neuropathy, immunological dysfunction, nutritional imbalance, and infection, to achieve more active therapeutic goals because of their engineering design and intelligent administration strategy. Furthermore, microneedle arrays have excellent biocompatibility and adaptable microstructure. Innovative dressings based on MAs are therefore expected to be used in wound healing more often in the future (Yao et al., 2022).
To conclude, it can be believed that MNs technology will bring many new thrilling breakthroughs in medical, healthcare, and biological applications and so the development of micro/nano manufacturing technology and more comprehensive studies on the corresponding mechanics’ problems concerning MNs are needed.
References
- Gidde, S. T. R., Ciuciu, A., Devaravar, N., Doracio, R., Kianzad, K., & Hutapea, P. (2020). Effect of vibration on insertion force and deflection of bioinspired needle in tissues. Bioinspiration & Biomimetics, 15(5), 054001. https://doi.org/10.1088/1748-3190/AB9341
- Jaffar-Bandjee, M., Casas, J., & Krijnen, G. (2018). Additive manufacturing: state of the art and potential for insect science. Current Opinion in Insect Science, 30, 79–85. https://doi.org/10.1016/J.COIS.2018.09.011
- Jana, B. A., & Wadhwani, A. D. (2019). Microneedle – Future prospect for efficient drug delivery in diabetes management. Indian Journal of Pharmacology, 51(1), 4. https://doi.org/10.4103/IJP.IJP_16_18
- Kim, J., Park, S., Nam, G., Choi, Y., Woo, S., & Yoon, S. H. (2018). Bioinspired microneedle insertion for deep and precise skin penetration with low force: Why the application of mechanophysical stimuli should be considered. Journal of the Mechanical Behavior of Biomedical Materials, 78, 480–490. https://doi.org/10.1016/J.JMBBM.2017.12.006
- Kim, Y. C., Park, J. H., & Prausnitz, M. R. (2012). Microneedles for drug and vaccine delivery. In Advanced Drug Delivery Reviews (Vol. 64, Issue 14, pp. 1547–1568). NIH Public Access. https://doi.org/10.1016/j.addr.2012.04.005
- Koh, K. J., Liu, Y., Lim, S. H., Loh, X. J., Kang, L., Lim, C. Y., & Phua, K. K. L. (2018). Formulation, characterization and evaluation of mRNA-loaded dissolvable polymeric microneedles (RNApatch). Scientific Reports, 8(1), 1–11. https://doi.org/10.1038/s41598-018-30290-3
- Ma, G., & Wu, C. (2017). Microneedle, bio-microneedle and bio-inspired microneedle: A review. In Journal of Controlled Release (Vol. 251, pp. 11–23). Elsevier B.V. https://doi.org/10.1016/j.jconrel.2017.02.011
- Microneedles for Painless Drug Delivery With Minimal Side Effects | Technology Networks. (n.d.). Retrieved July 18, 2022, from https://www.technologynetworks.com/drug-discovery/news/microneedles-for-painless-drug-delivery-with-minimal-side-effects-348486
- Plamadeala, C., Gosain, S. R., Hischen, F., Buchroithner, B., Puthukodan, S., Jacak, J., Bocchino, A., Whelan, D., Conor O’mahony, &, Baumgartner, W., & Heitz, J. (2019). Bio-inspired microneedle design for efficient drug/vaccine coating. https://doi.org/10.1007/s10544-019-0456-z
- Sharma, S., Hatware, K., Bhadane, P., Sindhikar, S., & Mishra, D. K. (2019). Recent advances in microneedle composites for biomedical applications: Advanced drug delivery technologies. Materials Science and Engineering: C, 103, 109717. https://doi.org/10.1016/J.MSEC.2019.05.002
- Waghule, T., Singhvi, G., Dubey, S. K., Pandey, M. M., Gupta, G., Singh, M., & Dua, K. (2019). Microneedles: A smart approach and increasing potential for transdermal drug delivery system. In Biomedicine and Pharmacotherapy (Vol. 109, pp. 1249–1258). Elsevier Masson SAS. https://doi.org/10.1016/j.biopha.2018.10.078
- Xu, J., Xu, D., Xuan, X., & He, H. (2021). Advances of microneedles in biomedical applications. Molecules, 26(19). https://doi.org/10.3390/molecules26195912
- Yao, S., Luo, Y., & Wang, Y. (2022). Engineered microneedles arrays for wound healing. Engineered Regeneration, 3(3), 232–240. https://doi.org/10.1016/J.ENGREG.2022.05.003
- Zhao, Z., Chen, Y., & Shi, Y. (2020). Microneedles: a potential strategy in transdermal delivery and application in the management of psoriasis. https://doi.org/10.1039/d0ra00735h
If you like this article, you can go through our other top articles
- A Short Overview of the Virulence Properties of Bacterial Enzymes- https://learnlifescience.com/a-short-overview-of-the-virulence-properties-of-bacterial-enzymes/
- BIOREMEDIATION: HOW IT WORKS- https://learnlifescience.com/bioremediation-how-it-works/
“Since the article has been written to reflect the actual views and capabilities of the author(s), they are not revised for content and only lightly edited to be confirmed with the Learn life sciences style guidelines.”








I must thank you for the efforts you have put in writing this blog. Im hoping to check out the same high-grade blog posts from you in the future as well. In fact, your creative writing abilities has encouraged me to get my own, personal site now 😉
An informative article. Hoping to get more from you .