Introduction
Monkeypox virus (MPXV), also known as Mpox, is an infectious double-stranded DNA virus. It is a zoonotic virus first identified in a captive monkey in a Danish research facility in 1958. The first human case was reported in a nine-year-old boy in the Democratic Republic of Congo in 1970. Since then, it has spread across Central, East, and West Africa, particularly during the 2022-2023 outbreaks. MPXV belongs to the Orthopoxvirus genus, which includes viruses such as smallpox, horsepox, cowpox, camelpox, vaccinia, and variola. MPXV has two subtypes: Clade I and Clade II. Clade II is further divided into Clade IIa and Clade IIb. Clade I is more virulent, though there have been no reported deaths associated with Clade II (World Health Organization, 2023). For over fifty years, MPXV was prevalent in central and western Africa, with limited spread to non-endemic areas. However, since 2017, MPXV has emerged in new regions outside of its endemic areas, leading to a significant outbreak in 2022 (Alakunle et al., 2024). Right now, monkeypox is a re-emerging viral threat and people should be aware of it.
Epidemiology
According to the WHO, Mpox was predominantly confined to the African subcontinent, especially in countries like the Democratic Republic of Congo, Nigeria, and Cameroon, until 2022. It has since spread to other regions, including Central America and Europe. The virus is transmitted from animals to humans through direct contact with blood, bodily fluids, or skin lesions of infected animals, or by consuming undercooked meat (Harris, 2022). Human-to-human transmission occurs via close contact with respiratory droplets, skin lesions, or contaminated materials. Vertical transmission from mother to fetus is also possible. Unlike previous outbreaks, the recent Mpox epidemic has been notably associated with sexual transmission, particularly among homosexual and bisexual men. One study reported that 98% of cases occurred in this demographic, with 41% also being HIV-positive. Furthermore, 73% of lesions were located in the anal and genital areas (Aden et al., 2023). The virus has an incubation period of 7 to 14 days, which may extend to 21 days. Symptoms typically last 14-21 days. MPXV can present with a wide range of symptoms, often resembling other common illnesses, which complicates accurate diagnosis.
Common Symptoms Include:
- Elevated temperature
- Severe headache
- Muscle aches, including back pain
- Swollen lymph nodes
- Shivering and chills
- Fatigue and lethargy
- Anal pain, often with bleeding
According to the WHO (2023), rashes or mucosal lesions typically appear within five days of the initial symptoms. These rashes often start on the face and then spread to other body parts, including the mouth and genitalia. The rash progresses from raised spots to pus-filled blisters, which eventually scab and fall off (NHS, 2024). The prolonged incubation period complicates early detection, leading to delayed medical intervention and an increased risk of transmission and severe complications. The severity of the disease varies depending on the strain. The Central African clade has a higher mortality rate, up to 10%, whereas the West African clade is less deadly, with a mortality rate of 1-3% (Mpox: What You Need to Know About the Latest Public Health Emergency, 2024).
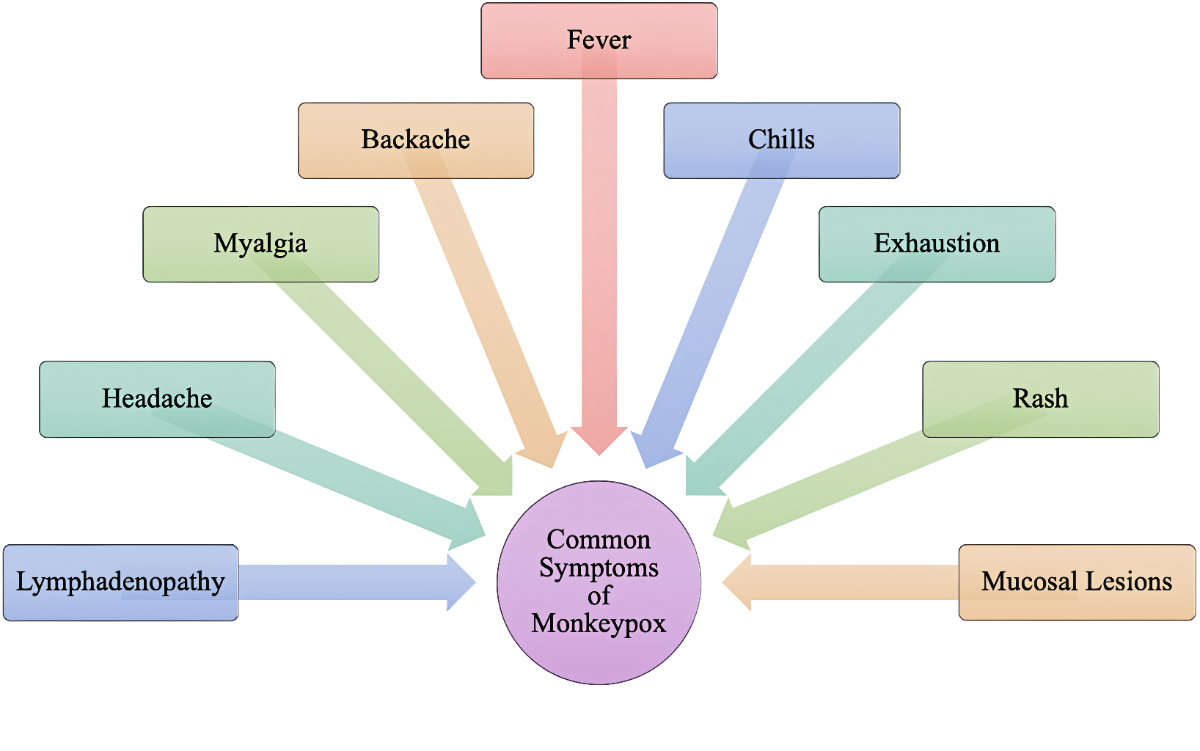
Figure 1: Clinical Conundrums: Differentiating Monkeypox From Similarly Presenting Infections. Image Courtesy: https://www.cureus.com/articles/113445-clinical-conundrums-differentiating-monkeypox-from-similarly-presenting-infections/
Transmission Routes
- Animal to Human (Zoonotic Transmission): MPXV is commonly found in wild rodents and monkeys in certain African regions. Transmission to humans can occur through bites, scratches, direct contact with an infected animal’s bodily fluids, or handling infected animals (Karan et al., 2023).
- Human to Human: Transmission can occur through direct contact with an infected person’s skin lesions, bodily fluids, or respiratory droplets. This includes intimate physical contact, such as touching, kissing, or sexual activity (Acharya et al., 2024).
- Maternal-Fetal Transmission: MPXV can be transmitted from an infected pregnant woman to her fetus, potentially leading to congenital Mpox (Karan et al., 2023).

Figure 2: Overview of Mpox transmission. Image courtesy: https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1132250/full
Global Risks
MPXV has mutated, posing a greater global health threat. It has been marked as one of the fastest-growing global health emergencies, with cases being reported daily in 2024. The rapid spread can be attributed to several factors, including close human contact, sexual transmission, particularly among homosexuals, limited vaccine availability, lack of public awareness, rapid virus mutation, and inadequate healthcare systems in underdeveloped countries. MPXV’s ability to spread across different animal species further complicates eradication efforts (WHO, 2024).
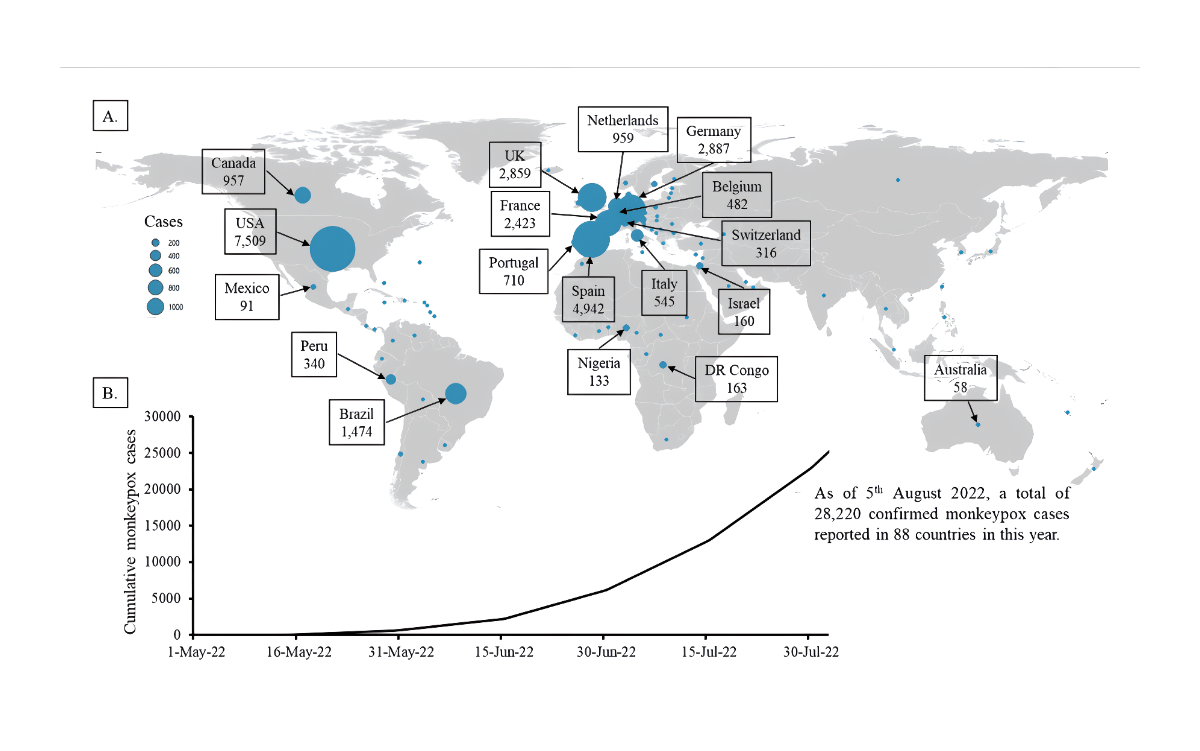
Figure 3: Unprecedented rise of monkeypox in Europe and America: Are Asian countries ready for a new outbreak during the ongoing COVID-19 pandemic? Image Courtesy: https://jogh.org/2022/jogh-12-03066/
Pathogenesis
MPXV can enter the body through various routes, including the upper respiratory tract (oropharynx and nasopharynx) and intradermal pathways (Sagdat et al., 2024). The virus binds to host cells via specific receptors, allowing it to enter the cells.
- Fusion: After attachment, MPXV enters host cells through macropinocytosis or direct fusion with the cell membrane. This fusion allows the viral envelope to merge with the host cell membrane, facilitating the entry of the viral core into the cytoplasm (Martínez-Fernández et al., 2023).
- Replication: Once inside the host cell, MPXV replicates its double-stranded DNA in the cytoplasm. Viral factories are formed at specific sites for the production of viral proteins, which are essential for virus replication and immune response regulation. MPXV produces two infectious forms: Intracellular Mature Virus (IMV) and Extracellular Enveloped Virus (EEV). IMVs are released upon cell lysis and remain stable in the environment, while EEVs are synthesized in the Golgi body and released by exocytosis, facilitating cell-to-cell dissemination and evasion of the host immune response.
- Release: Newly formed viruses accumulate in the cytoplasm. IMVs are released after cell lysis, while EEVs exit the cell through budding or actin tail assembly, enabling the virus to spread to surrounding cells.

Figure 4: A schematic overview of the MPXV life cycle. Image courtesy: https://www.mdpi.com/2076-0817/12/7/947
Diagnostics
The WHO and CDC recommend real-time PCR as the most effective diagnostic method for Mpox in humans and animals. Numerous real-time PCR assays targeting different parts of the MPXV genome have been developed since the virus’s emergence (Da Silva et al., 2023).
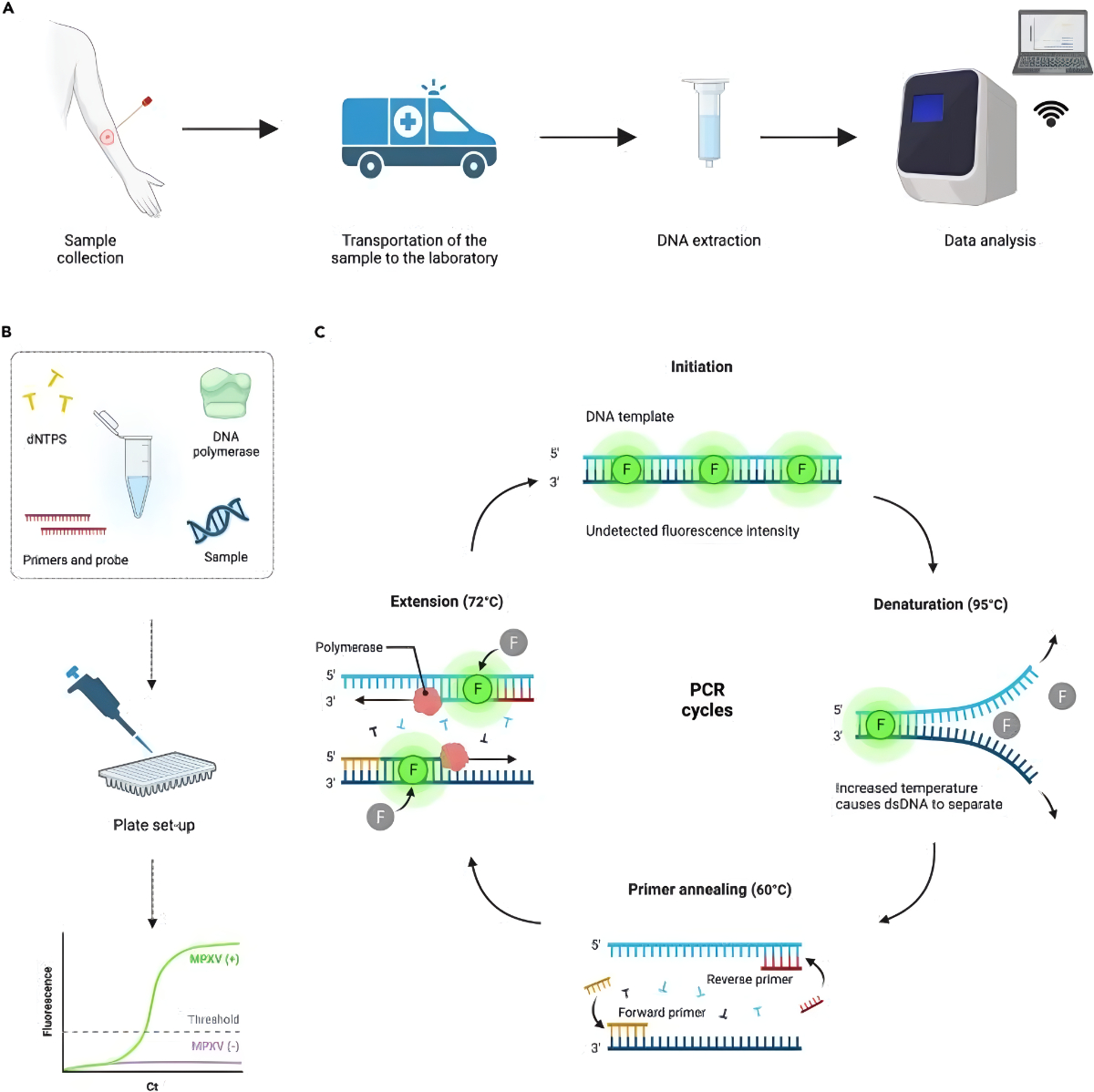
Figure 5: Real-time PCR workflow for MPXV detection. Image courtesy: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10183700/
Immunization
MVA-BN (Modified Vaccinia Ankara – Bavarian Nordic) is a third-generation smallpox vaccine marketed under the brand names Jynneos, Imvanex, or Imvamune. It is a live attenuated, non-replicating vaccine effective against Mpox and smallpox. The vaccine is recommended for individuals aged 18 and over who are at higher risk. It is administered in two doses, four weeks apart, with research indicating that even a single dose provides some protection. A third dose may further enhance the immune response (Zaeck et al., 2022).
- Effectiveness: MVA and MPXV belong to the Orthopoxvirus genus, sharing considerable genomic similarities. Studies have shown that MVA-BN vaccination induces antibodies that neutralize both MVA and MPXV, making the vaccine effective in preventing MPXV infection (Gao et al., 2023).
- Safety and Prevention: Prevention of Mpox involves rigorous sanitation protocols, including frequent handwashing, maintaining hygiene during food preparation, and physical distancing from suspected carriers. Sexual risk reduction, early detection, and quarantine are also crucial. Individuals with recognizable symptoms should seek medical attention immediately and isolate themselves to prevent virus transmission (Mpox, 2024).

Figure 6: Monkeypox vaccine. Image Courtesy: https://pink.citeline.com/PS146407/EMA-Reviewing-Bavarian-Nordics-Imvanex-For-Vaccination-Against-Monkeypox

Figure 7: The Preventive measures of Mpox. Image Courtesy: https://studenthealth.ucsd.edu/resources/health-topics/monkeypox/index.html
Treatment
Mpox treatment requires close monitoring and includes symptomatic treatment with over-the-counter pain relievers, such as acetaminophen and ibuprofen. Tecovirimat (TPOXX), an FDA-approved antiviral initially developed for smallpox, has shown promise in treating severe Mpox cases. However, it is currently available only through clinical trials (CDC, 2024). Isolation and appropriate wound care are essential to prevent secondary infections and virus transmission.
Conclusion
The re-emergence of monkeypox as a global health threat highlights the need for heightened awareness, surveillance, and research. While historically confined to certain regions in Africa, the recent outbreaks have demonstrated the virus’s ability to spread widely, facilitated by close human contact and the evolution of transmission routes, including sexual transmission. Effective diagnostic methods, such as real-time PCR, and the availability of vaccines like MVA-BN, offer hope in controlling the spread of the virus. However, the rapid mutation of the virus and the lack of widespread vaccine distribution underscore the ongoing challenges in managing this public health crisis. Continued vigilance, public education, and international collaboration are essential to mitigate the impact of monkeypox and prevent future outbreaks.
References
- Acharya, A., Kumar, N., Singh, K., & Byrareddy, S. N. (2024). “MPOX in MSM: Tackling stigma, minimizing risk factors, exploring pathogenesis, and treatment approaches.” Biomedical Journal, 100746. https://doi.org/10.1016/j.bj.2024.100746
- Aden, D., Zaheer, S., Kumar, R., & Ranga, S. (2023). Monkeypox (Mpox) outbreak during COVID‐19 pandemic—Past and the future. Journal of Medical Virology, 95(4). https://doi.org/10.1002/jmv.28701
- Alakunle, E., Kolawole, D., Diaz-Cánova, D., Alele, F., Adegboye, O., Moens, U., & Okeke, M. I. (2024). A comprehensive review of monkeypox virus and mpox characteristics. Frontiers in Cellular and Infection Microbiology, 14. https://doi.org/10.3389/fcimb.2024.1360586
- Da Silva, S. J. R., Kohl, A., Pena, L., & Pardee, K. (2023). Clinical and laboratory diagnosis of monkeypox (mpox): Current status and future directions. iScience, 26(6), 106759. https://doi.org/10.1016/j.isci.2023.106759
- Gao, F., He, C., Liu, M., Yuan, P., Tian, S., Zheng, M., Zhang, L., Zhou, X., Xu, F., Luo, J., & Li, X. (2023). Cross-reactive immune responses to monkeypox virus induced by MVA vaccination in mice. Virology Journal, 20(1). https://doi.org/10.1186/s12985-023-02085-0
- Harris, E. (2022). What to know about Monkeypox. JAMA, 327(23), 2278. https://doi.org/10.1001/jama.2022.9499
- How to protect yourself | MPOX | Poxvirus | CDC. (n.d.). https://www.cdc.gov/poxvirus/mpox/prevention/protect-yourself.html
- Idris, S. (2024, August 15). MPOX PREVENTION: NCDC issues alerts. Nigerian Television Authority – Africa’s Largest TV Network. https://nta.ng/2024/08/15/mpox-prevention-ncdc-issues-alerts/
- Karan, A., Contag, C. A., & Pinksy, B. (2023). Monitoring routes of transmission for human mpox. The Lancet, 402(10402), 608–609. https://doi.org/10.1016/s0140-6736(23)01131-5
- Lu, J., Xing, H., Wang, C., Tang, M., Wu, C., Ye, F., Yin, L., Yang, Y., Tan, W., & Shen, L. (2023). Mpox (formerly monkeypox): pathogenesis, prevention, and treatment. Signal Transduction and Targeted Therapy, 8(1). https://doi.org/10.1038/s41392-023-01675-2
- Lum, F., Torres-Ruesta, A., Tay, M. Z., Lin, R. T. P., Lye, D. C., Rénia, L., & Ng, L. F. P. (2022). Monkeypox: disease epidemiology, host immunity and clinical interventions. Nature Reviews. Immunology, 22(10), 597–613. https://doi.org/10.1038/s41577-022-00775-4
- Martínez-Fernández, D. E., Fernández-Quezada, D., Casillas-Muñoz, F. a. G., Carrillo-Ballesteros, F. J., Ortega-Prieto, A. M., Jimenez-Guardeño, J. M., & Regla-Nava, J. A. (2023). Human Monkeypox: A Comprehensive overview of epidemiology, pathogenesis, diagnosis, treatment, and prevention strategies. Pathogens, 12(7), 947. https://doi.org/10.3390/pathogens12070947
- Mpox. (2024, May 1). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22371-monkeypox
- Mpox Vaccine Safety. (2024, July 31). Vaccine Safety. https://www.cdc.gov/vaccine-safety/vaccines/mpox.html
- Mpox: What you need to know about the latest public health emergency. (2024, August 20). UN News. https://news.un.org/en/story/2024/08/1153361
- Patient’s Guide to Mpox Treatment with Tecovirimat (TPOXX) | Mpox | Poxvirus | CDC. (n.d.). https://www.cdc.gov/poxvirus/mpox/if-sick/treatment.html
- Public Health Agency of Canada. (2024, March 26). Mpox: How it spreads, prevention and risks. Canada.ca. https://www.canada.ca/en/public-health/services/diseases/mpox/risks.html
- Sagdat, K., Batyrkhan, A., & Kanayeva, D. (2024). Exploring monkeypox virus proteins and rapid detection techniques. Frontiers in Cellular and Infection Microbiology, 14. https://doi.org/10.3389/fcimb.2024.1414224
- Toth, A. (2024, August 21). Mpox virus mapped: Which countries has the new virus strain spread to? The Independent. https://www.independent.co.uk/news/health/mpox-outbreak-map-sweden-pakistan-uk-b2598210.html
- World Health Organization: WHO & World Health Organization: WHO. (2023, April 18). Mpox (monkeypox). https://www.who.int/news-room/fact-sheets/detail/monkeypox
- Zaeck, L. M., Lamers, M. M., Verstrepen, B. E., Bestebroer, T. M., Van Royen, M. E., Götz, H., Shamier, M. C., Van Leeuwen, L. P. M., Schmitz, K. S., Alblas, K., Van Efferen, S., Bogers, S., Scherbeijn, S., Rimmelzwaan, G. F., Van Gorp, E. C. M., Koopmans, M. P. G., Haagmans, B. L., GeurtsvanKessel, C. H., & De Vries, R. D. (2022). Low levels of monkeypox virus-neutralizing antibodies after MVA-BN vaccination in healthy individuals. Nature Medicine, 29(1), 270–278. https://doi.org/10.1038/s41591-022-02090-w
If you like this article, you can go through our other top articles
- Phytoremediation: A Potential Candidate for Environmental Catharsis- https://learnlifescience.com/phytoremediation-a-potential-candidate-for-environmental-catharsis/
- A Comprehensive Review of Thalassemia- https://learnlifescience.com/a-comprehensive-review-of-thalassemia/
- DNA Sequencing Methods – https://learnlifescience.com/dna-sequencing-methods/
- An Overview of Bacterial Genomic DNA Isolation – https://learnlifescience.com/an-overview-of-bacterial-genomic-dna-isolation/
“Since the article has been written to reflect the actual views and capabilities of the author(s), they are not revised for content and only lightly edited to be confirmed with the Learn life sciences style guidelines”








Your blog is like a beacon of light in the vast expanse of the internet. Your thoughtful analysis and insightful commentary never fail to leave a lasting impression. Thank you for all that you do.